
BlockCamp: A One-Day Boot Camp to Teach Ultrasound Guided Nerve Blocks
Ariella Cohen, MD, PYG3 Resident, Department of Emergency Medicine, Maimonides Medical Center
Alyssa Nguyen-Phuoc, MD, Ultrasound Faculty, Department of Emergency Medicine, Maimonides Medical Center
Judy Lin, MD, FACEP, Director of Emergency Ultrasound, Institutional GME Ultrasound Director, Assistant Professor, Department of Emergency Medicine, Baylor Scott & White All Saints, Fort Worth, TX
Kay Odashima, MD, Ultrasound Faculty, Department of Emergency Medicine, Maimonides Medical Center
Amy Sanghvi, MD, Ultrasound Faculty, Department of Emergency Medicine, Maimonides Medical Center
Lawrence Haines, MD, MPH, RDMS, FACEP, Ultrasound Division Director, Department of Emergency Medicine, Maimonides Medical Center; Assistant Professor, Emergency Medicine, SUNY Downstate Health Sciences University
Leily Naraghi, MD, FACEP, Ultrasound Fellowship Director, Department of Emergency Medicine, Maimonides Medical Center, Assistant Professor, Emergency Medicine, SUNY Downstate Health Sciences University (lead/corresponding author)
@MaimoUltrasound
Background
In the setting of an ongoing opioid epidemic, alternative modalities for pain management have become popular in the emergency department (ED). One example is the use of ultrasound guided regional anesthesia or nerve blocks for pain control in various injuries and procedures such as chest tube insertion, laceration repairs, and joint reductions. Ultrasound guidance for nerve blocks have become the new standard of care as ultrasound guidance has improved success and decreased complication rates of these procedures.1
Despite the value of ultrasound guided nerve blocks, the implementation of them in the emergency setting has been limited. One obstacle is the lack of routine training of ultrasound guided nerve blocks, for both faculty and residents. Emergency ultrasound is integral to the practice of emergency medicine, and it is standard across Emergency resident education. Integrating education of ultrasound guided regional anesthesia into an already existing ultrasound curriculum would increase proficiency of learners.1
While many academic EDs are beginning to utilize ultrasound guided regional anesthesia, there is inconsistency in training, practice and policy among them.2 A cross-sectional study conducted by Wilson et al. highlighted that a large barrier to the practice of ultrasound guided regional anesthesia was lack of formal training or dissatisfaction with the level of training among faculty.3 In an attempt to remedy this problem, the Maimonides Medical Center Emergency Ultrasound Division in Brooklyn, NY designed and launched “BlockCamp,” a one-day ultrasound guided nerve block course.
What is BlockCamp?
This course is a regional nerve block conference held by the Maimonides Medical Center Emergency Medicine Ultrasound Division. It was held in 2020, 2022 and in May 2023. The course is a one-day intensive that consists of three portions: lecture-based didactics, ultrasounding live anatomy models, and practicing injections on high fidelity simulated meat models. Didactic lectures explore the most commonly performed blocks in the Emergency Department, as well as reviewing topics such as the local anesthetic types, correct dosing and toxicity. Participants practice identifying external landmarks and sonoanatomy on live models4. Participants then have the opportunity to practice ultrasound guided injections on high fidelity meat models. The models are reusable and allow participants to practice in-line technique and visualize how infiltration of saline appears under ultrasound.4 (Image 1, 2 and video 1). Identification of external landmarks and sonoanatomy are also practiced on live models. Participants rotate through stations until they complete all available models. A broad range of physicians from all levels of training - residents, fellows and attendings - participate in this program.
The Study
A study was performed at BlockCamp 2022 to assess both the short term and long-term efficacy of BlockCamp. Participants were asked to fill out short quizzes at the beginning of each lecture. At the end of BlockCamp, participants filled out another quiz, which was a composite of all quiz questions in an attempt to measure course effectiveness and short-term recall. These questions were emailed to participants 90 days later to assess their long-term recall. Data gathered from these quizzes was analyzed to determine knowledge acquisition and retention. Of the fifty participants in BlockCamp, forty subjects completed knowledge assessments prior to the intervention, thirty-nine after intervention, and fifteen completed a 90-day follow-up assessment. There was a significant improvement in knowledge assessment immediately following BlockCamp that was not sustained over time. This data suggests that continuing education is necessary to maintain both comfort with the procedure and mastery of key concepts.
The Future
Looking forward, we hope to expand BlockCamp further. Each year, surveys are gathered at the end of the course in order to get participant feedback. This feedback is implemented when organizing and planning future sessions. This year’s conference, for example, will be offered twice on two consecutive days rather than just once, incorporating feedback suggesting that a single session did not allow for enough participants to attend. We also aim to expand these sessions to a national, rather than regional, audience. In 2022, participants traveled from five different states to attend the workshop, and additional programs will be joining us for 2023. Lastly, as new applications of ultrasound guided nerve blocks are being studied and used, we hope to incorporate them into future BlockCamp sessions.
Teaching physicians skills and techniques of nerve blocks will add to their scope of treatment for patients that present to the Emergency Department in acute or chronic pain. The other advantage to BlockCamp is that most current emergency medicine (EM) focused regional anesthesia courses exist in conjunction with a conference, which requires more monetary investment. Being able to purchase these courses individually helps to make this affordable, and potentially something that learners can participate in yearly to help with knowledge retention. Other standalone ultrasound guided nerve block courses are generally organized by non-EM specialties and may include info not as applicable to EM.
Our hope is that the BlockCamp participants will not only improve their clinical practice but also become comfortable with the techniques so that they can teach these skills to their peers. The ultimate goal of BlockCamp is to increase utilization of ultrasound guided nerve blocks and decrease the utilization of systemic opioids in the face of our national crisis.
References
- Wilson C. Feeling blocked? Another pain management tool in the emergency department. Ann Emerg Med. 2018;72(2):120-6.
- Amini R, Kartchner JZ, Nagdev A, Adhikari S. Ultrasound‐guided nerve blocks in emergency medicine practice. J Ultrasound Med. 2016;35(4):731-6.
- Wilson CL, Chung K, Fong T. Challenges and variations in emergency medicine residency training of ultrasound‐guided regional anesthesia techniques. AEM Education and Training. 2017;1(2):158-64.
- Naraghi L, Lin J, Odashima K, Buttar S, Haines L, Dickman E. Ultrasound-guided regional anesthesia simulation: use of meat glue in inexpensive and realistic nerve block models. BMC Medical Education. 2019;19(1):1-10.
 Image 1- Meat model simulating the supraclavicular brachial plexus.
Image 1- Meat model simulating the supraclavicular brachial plexus.
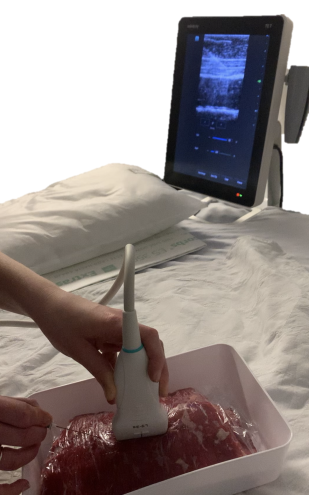 Image 2. Meat model simulating transverse abdominis plane block.
Image 2. Meat model simulating transverse abdominis plane block.
Video 1. Simulation of hydrodissection with saline injection in a fascia iliaca block model. https://youtu.be/BNb5TJOtX7Q


