When the X-ray is Negative: Using POCUS to Increase Diagnostic Accuracy in Acute Knee Pain
From the System-Wide Clinical Ultrasound Directors Subcommittee of the ACEP Emergency Ultrasound Section
Case Presentation
A 55-year-old man presents to the emergency department with right knee pain. He was seen three days prior for the same complaint, and had a negative three-view X-ray at that time. A sunrise view was not obtained. He reports that approximately two weeks ago he “twisted” his knee while moving furniture but denies falling or other direct trauma. His past medical history includes hypertension and moderate obesity; his estimated BMI is 31. He reports that he contracted and recovered from COVID-19 in December of 2019, and has had occasional residual shortness of breath, but denies current fevers, joint swelling, or skin changes. He is ambulatory in the ED, but his knee pain is unchanged. What are your next steps?
Discussion and Role of POCUS
Joint pain is among the most common chronic complaints in U.S. adults, afflicting approximately a quarter of the population and accounting for 20% of current annual primary care and emergency department visits.1,2 For those reporting knee pain, increasing trends in age and obesity account for some, but not all of the increase in complaints seen in the past two decades.3 While the common diagnostic approach to the evaluation of knee pain often includes a radiograph, significant variability exists in the correlation of pain and positive findings, ranging from 15-81%.4 For adults with suspected fracture, radiography demonstrates 100% sensitivity when used with a common clinical decision rule such as the Ottawa Knee rule.5 An X-ray is recommended if any of the following criteria are present: Age > 55, tenderness to palpation over fibular head or isolated over the patella, inability to flex to 90 degrees, or inability to walk after taking 4 steps in the emergency department.6 In absence of trauma and with recent negative radiography, attention must be turned to non-radiographic pathology. Bedside clinical ultrasound is a high-yield diagnostic tool for both emergency providers and those practicing office-based medicine, and is useful in diagnostic time reduction, in resource-limited environments, and in times when radiography is non-diagnostic.7
Using the high-frequency linear probe, typical views are obtained superior and inferior to the patella, as well as medial, lateral, and posterior to the knee joint. Views superior and inferior to patella assess for the integrity of the quadriceps and patellar tendons, the patella, as well as presence of knee effusion. Normal examination of the overlying skin and absence of cobblestoning of the soft tissue on ultrasound lessens the likelihood of cellulitis and abscess. Figure 1 shows the anterior ultrasound view of the knee, the patella. An intact patella should demonstrate the uninterrupted hyperechoic curvature of the cortical surface. In figure 1, we see an unmistakable cortical disruption (between the two red arrows), indicating a patellar fracture. Knee effusions will appear as an anechoic collection, indicated by the blue arrow, deep to the tendons. (Fig. 2) Medial and lateral views can also demonstrate effusions. Complex effusions such as hemarthrosis appear as hypoechoic collections if clotting has occurred. Figure 3 demonstrates a traumatic hemarthrosis identified by the green arrow. Figure 4 shows another simple knee effusion, indicated by the green arrow, without a history of trauma. Aspiration in the emergency department or office can be useful in directing therapy. In Figure 4, we see the needle approaching the effusion from the left side of the screen highlighted by the red arrow. Lastly, the posterior aspect of the knee contains the popliteal vessels. The popliteal vessels should be identified by Color Doppler, allowing differentiation from the non-vascular structures. Figure 5 shows a cystic non-compressible, anechoic structure without internal echoes within the popliteal fossa highlighted by the yellow arrow.
Clinical Course
The patient declined a repeat X-ray from triage, citing concerns that his insurance would deny a second study. A bedside ultrasound was performed instead, demonstrating a moderate knee effusion, and assisting in needle localization in this gentleman with a BMI >30. Negative birefringent crystals were noted on lab analysis, confirming a suspected diagnosis of gout, with recommendation for NSAIDS and a short course of oral steroids. The patient was discharged in less than average time and reported satisfaction with his care.
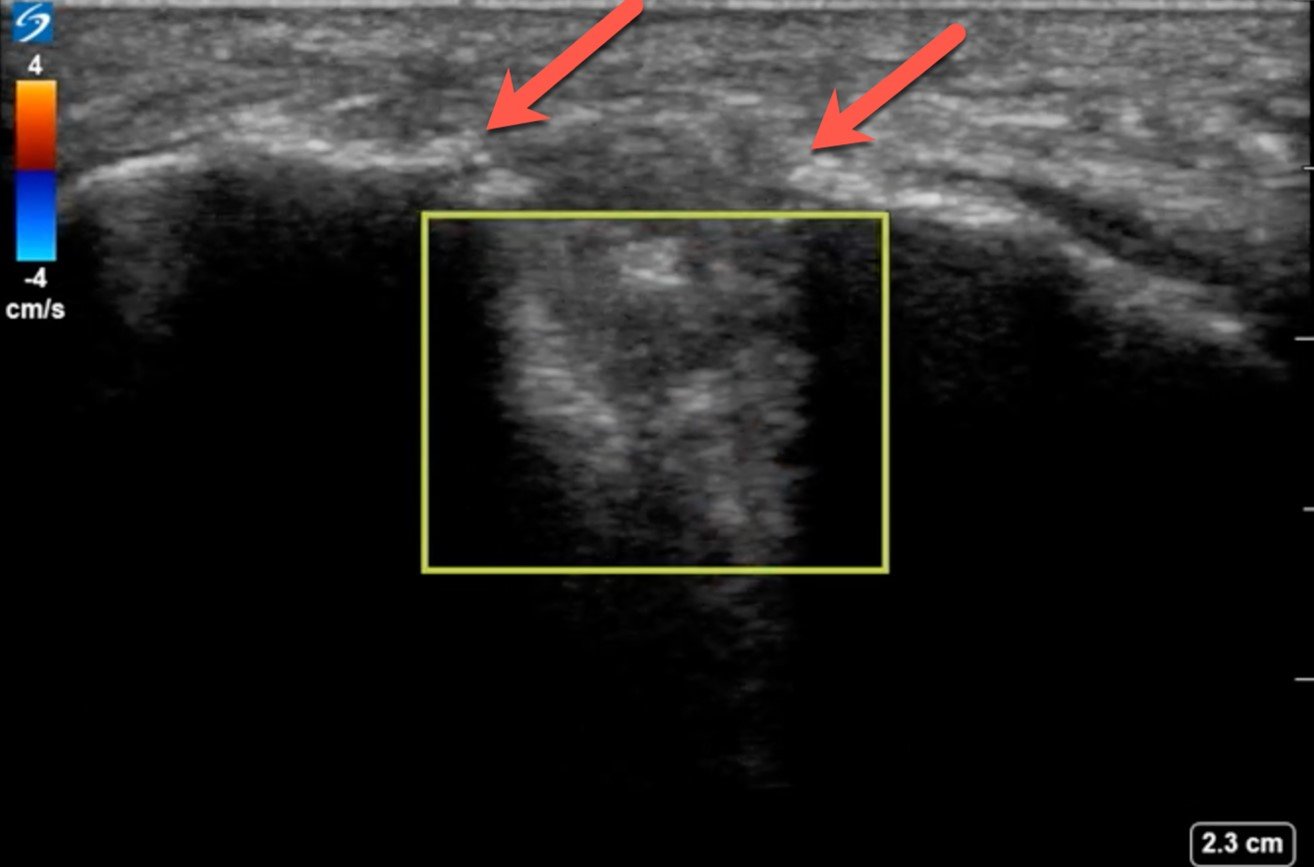
Figure 1

Figure 2
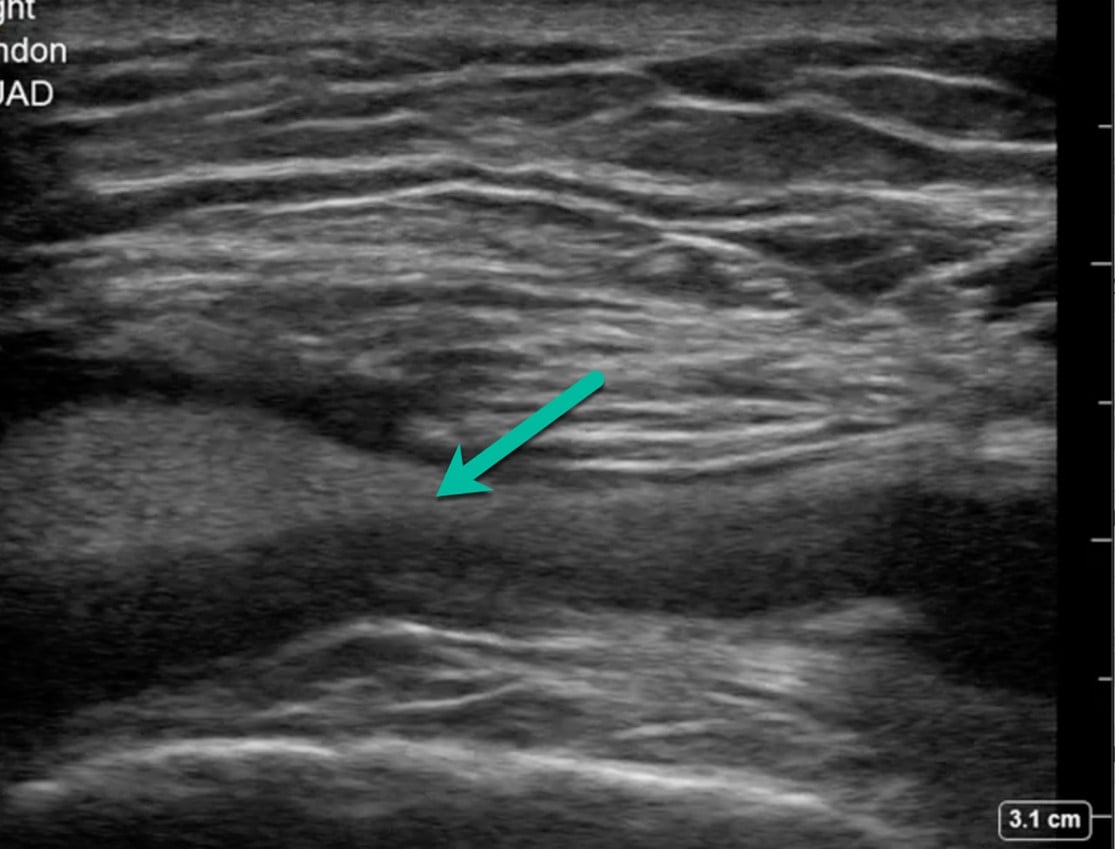
Figure 3
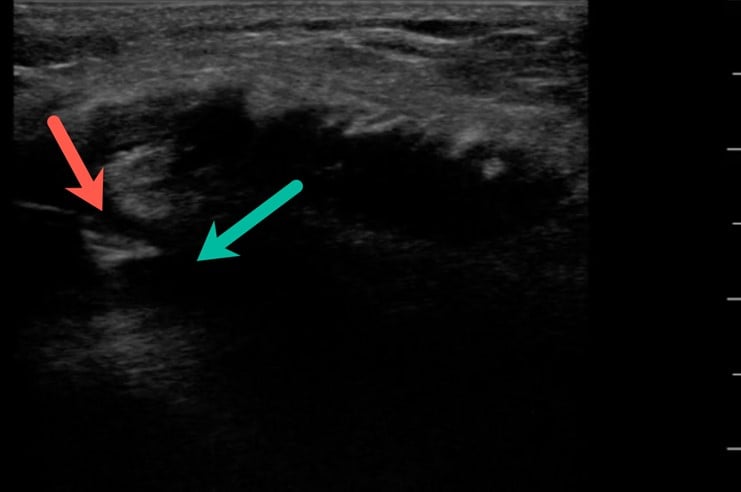
Figure 4
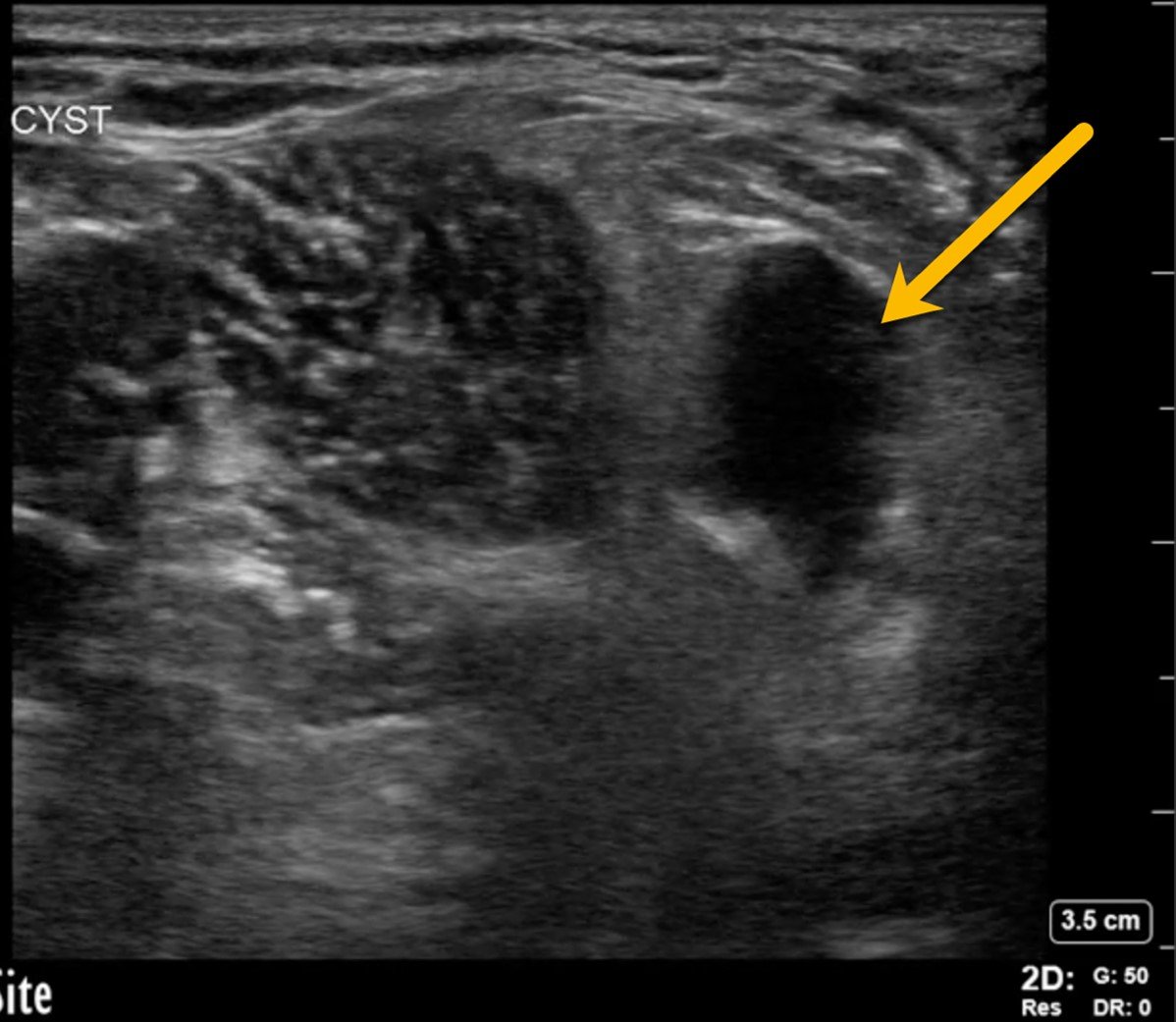
Figure 5
References
- Barbour KE, Boring M, Helmick CG, et al. Prevalence of severe joint pain among adults with doctor-diagnosed arthritis—United States, 2002–2014. MMWR Morb Mortal Wkly Rep. 2016;65(39):1052–6.
- Miller AN. Evaluation of common musculoskeletal injuries in the urgent setting. MedEdPORTAL. 2016;12:10514.
- Nguyen US, Zhang Y, Zhu Y, et al. Increasing prevalence of knee pain and symptomatic knee osteoarthritis: survey and cohort data. Ann Intern Med. 2011;155(11):725-732.
- Bedson J, Croft PR. The discordance between clinical and radiographic knee osteoarthritis: a systematic search and summary of the literature. BMC Musculoskelet Disord. 2008;9:116. Published 2008 Sep 2.
- Stiell IG, Greenberg GH, Wells GA, et al. Prospective validation of a decision rule for the use of radiography in acute knee injuries. 1996;275(8):611-615.
- Stiell IG, Greenberg GH, Wells GA, et al. Derivation of a decision rule for the use of radiography in acute knee injuries. Ann Emerg Med. 1995;26(4):405-413.
- Sippel S, Muruganandan K, Levin A, et al. Review article: Use of ultrasound in the developing world. Int J Emerg Med. 2011;4:72
Amie H. Woods, MD, FACEP
Director, Point of Care Ultrasound Inova Fairfax Emergency Department; Chair, System-wide QA Committee for POCUS Inova Health System, Falls Church, VA
Robert Strony, DO, MBA, CRC, FACEP
Medical Director, Point of Care Ultrasound; Director, Provider Network Management and Strategy Geisinger Health Plan, Danville PA
Zachary P. Soucy, DO, FACEP
Director, Emergency Department Ultrasound; Co-Chair system-wide Point of Care Ultrasound Committee Dartmouth-Hitchcock Medical Center, Lebanon, NH