
Cases that Count: Serial FAST examinations in a patient with a penetrating stab wound to the buttock
Case Presentation:
An 18-year-old male was brought in by EMS with a penetrating stab wound to his left buttock from an unknown weapon. Blood was oozing from the stab wound entry site, but he was hemodynamically stable. Shortly after arrival to the emergency department, he developed frank hematuria. An initial FAST exam revealed a large clot within the bladder walls (Fig. 1) but was negative for intraabdominal free fluid. A large hematuria catheter was placed by Urology to evacuate this clot. CT and CT angiogram of the abdomen and pelvis revealed active bleeding within and adjacent to the left posterior bladder wall, as well as a clot filled bladder and a deep pelvic hematoma displacing the rectum. A CT cystogram revealed no filling defect within the distal ureters or extravasation of contrast to suggest intra- or extra-peritoneal bladder rupture. After CT imaging, Urology copiously irrigated the bladder with normal saline to remove the clot. During irrigation, the patient developed significant abdominal pain and distension. A repeat FAST exam was performed revealing free fluid in the right upper quadrant (Fig. 2), left upper quadrant (Fig. 3), and pelvis (Fig. 4). The pelvic view also revealed an enhanced peritoneal stripe sign (Fig. 4) suggesting pneumoperitoneum.
Importance, Utility, and Accuracy of the Focused Assessment with Sonography for Trauma (FAST)
Trauma is the leading cause of adolescent mortality in the developed world.1 While blunt injury mechanisms predominate, penetrating trauma accounts for up to 20% of all trauma cases in the pediatric/ adolescent population.2 The purpose of the FAST exam is to detect clinically significant free intraabdominal fluid, usually representing blood in trauma victims, that requires operative intervention. However, other intra-abdominal fluid, such as urine from a ruptured bladder, can appear identical to blood in the FAST exam.3 Numerous studies have examined the accuracy of the FAST in detecting free abdominal fluid in adult trauma patients, with sensitivities ranging between 85-100% and specificities between 95-100% consistently reported for the hypotensive trauma patient.4,5 The FAST exam is more accurate ruling in than ruling out intra-abdominal injury. It is important to note that the FAST may be less sensitive in penetrating abdominal trauma (ranging from 50-70%) and in hemodynamically stable patients or those with minor trauma.5 The accuracy of the FAST exam in pediatric patients is less well described, with wider ranges of sensitivity and specificity reported. A meta-analysis showed a pooled sensitivity of 80% and specificity of 96% for identification of hemoperitoneum in pediatric blunt trauma patients.6 FAST has also been shown to significantly impact patient care by decreasing time to disposition, time to operative intervention, length of hospital stay, total cost, and number of CT scans performed (which is especially important in the pediatric population).7 The FAST exam is now a key element incorporated into most adult trauma algorithms as an adjunct to the primary survey, to be repeated when clinically indicated, and has become standard of care.5,8
Technique Tips
The sonographic question to answer when performing the FAST exam is: “Is there free fluid in the peritoneum or pericardium?” The enhanced FAST (eFAST), includes evaluation of the pleural space for hemothorax and pneumothorax as well. FAST can detect as little as 250 mL of peritoneal free fluid which would appear anechoic.9 However, it is important to note that delayed presentations with clotted blood may appear hyperechoic.
Ten structures/ spaces should be visualized through 4 acoustic windows:
- Right upper quadrant (RUQ): Morrison’s pouch (hepatorenal recess), liver tip (right paracolic gutter), and the lower right thorax.
- Left upper quadrant (LUQ): subphrenic space, splenorenal recess, spleen tip (left paracolic gutter), and the left lower thorax.
- Suprapubic: rectovesical pouch in male patients, rectouterine pouch (Pouch of Douglas) in female patients.
- Cardiac (most often subxiphoid, though other views may be obtained): pericardium and heart chambers (especially the right ventricle).
A low frequency curvilinear (2-5MHz) or phased array (2-8MHz) transducer may be used, and a high frequency linear (5-10 MHz) transducer may be used for higher resolution images in small children.10 The patient should be in the supine position. Placing the patient in 5-10 degrees of Trendelenburg will increase the sensitivity of detecting free fluid and may decrease the amount of free fluid necessary for a positive FAST exam.
The evaluation of adult patients usually starts with the RUQ view, since this is the location that free fluid collects first, followed by the LUQ view. If there is difficulty identifying structures or spaces in the upper abdominal views, have the patient inhale deeply which may help bring the liver/spleen/heart down into view rather than looking through intercostal spaces with the effect of rib shadowing. It is important to visualize both kidneys in their entirety as blood may collect only at the inferior or superior poles. A more posterior placement of the probe may be necessary to aim towards the kidneys to obtain a complete view. In the suprapubic view, free fluid may be visualized either posterior or adjacent to the bladder. It is often necessary to decrease the far field gain (time gain compensation) to minimize posterior acoustic enhancement artifact and improve visualization of free fluid. Fluid in the bladder optimizes this view, and an empty bladder may make it difficult to assess the suprapubic area for free fluid. In addition, a Foley catheter may make it difficult to distinguish the bladder from surrounding free intraperitoneal fluid. (Fig. 4) In younger patients, consider starting with the suprapubic view, as this is the most dependent portion of the abdominal cavity in children.
A FAST exam may be falsely negative when performed early in the patient’s course because there has not been enough time for sufficient fluid to accumulate. Repeating the FAST at intervals as well as anytime the patient’s condition changes (ie, hemodynamic status, development of new symptoms), will increase its overall sensitivity.11 The FAST exam is not intended to quantify the amount of intra-peritoneal fluid. Results should only be interpreted in the context of the patient’s specific clinical scenario and condition.
The enhanced peritoneal stripe sign (EPSS)
The EPSS has been described as a specific sonographic sign of pneumoperitoneum. The peritoneal stripe is normally seen as a thin echogenic line at the interface of the anterior abdominal wall and adjacent intraperitoneal fluid. In patients with pneumoperitoneum, small amounts of free air produce focal enhancement and apparent thickening of the peritoneal stripe (EPSS). (Fig. 4) Larger amounts of air may produce both the EPSS as well multiple reverberation artifacts, appearing as horizontal stripes and echogenic lines with comet tails.12,13
Clinical Course
The patient was brought for emergency diagnostic angiography and laparoscopy. Two full thickness injuries to the bladder (lateral and at the dome) were identified along with a large amount of irrigation fluid in the abdomen. The injuries were repaired, and a ureteral stent and a Foley catheter were placed. No other intraperitoneal injuries were identified. The patient was discharged home on post-operative day 4, and he underwent a successful trial of void and ureteral stent removal 1 week later.
This case demonstrates the importance of the FAST examination, both as part of the primary trauma survey and as serial repeat FAST exams when the clinical condition changes (in this case, development of abdominal pain with bladder irrigation). This repeat FAST exam allowed for expedited definitive diagnosis and management for our patient.
Figures
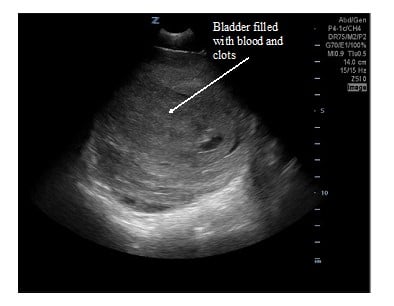
Figure 1. Transverse suprapubic view of the initial FAST. A well-circumscribed structure with mixed echogenicity is seen, which is the bladder filled with blood and clots.
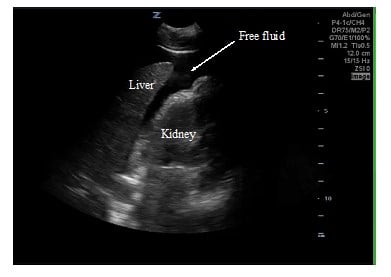
Figure 2. RUQ view of the repeat FAST. Anechoic free fluid is seen in Morrison’s pouch and surrounding the tip of the liver.
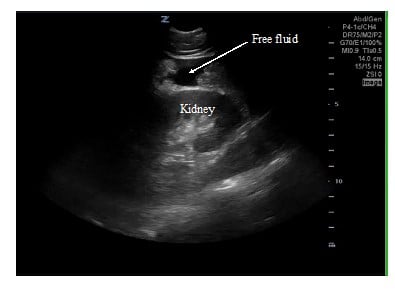
Figure 3. LUQ view of the repeat FAST. Anechoic free fluid is seen at the inferior pole of the kidney and at the spleno-renal recess.
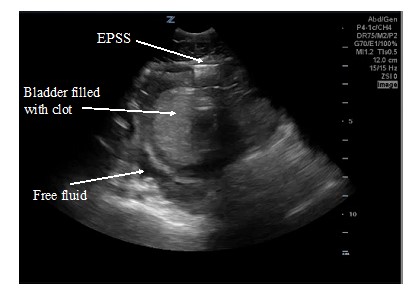
Figure 4. Pelvic view of the repeat FAST. Free intraperitoneal air is seen as the enhanced peritoneal stripe sign (EPSS). Anechoic free fluid is also seen posterior to the bladder.
References
- Shaw KN, Bachur RG, eds. Fleisher & Ludwig’s Textbook of Pediatric Emergency Medicine. 7th edition. Wolters Kluwer; 2016.
- Cotton BA, Nance ML. Penetrating trauma in children. Semin Pediatr Surg. 2004;13(2):87-97.
- Doniger, Stephanie J. Pediatric Emergency Critical Care and Ultrasound. Cambridge University Press; 2014.
- Stengel D, Leisterer J, Ferrada P, et al. Point-of-care ultrasonography for diagnosing thoracoabdominal injuries in patients with blunt trauma. Cochrane Injuries Group, ed. Cochrane Database of Systematic Reviews. Published online December 12, 2018.
- Atkinson P, Bowra J, Harris T, et al. Point-of-Care Ultrasound for Emergency Medicine and Resuscitation. 2019.
- Holmes JF, Gladman A, Chang CH. Performance of abdominal ultrasonography in pediatric blunt trauma patients: a meta-analysis. J Pediatr Surg. 2007;42(9):1588-94.
- Ultrasound Guidelines: Emergency, point-of-care and clinical ultrasound guidelines in medicine. Ann Emerg Med. 2017;69(5):e27-e54.
- American College of Surgeons, Committee on Trauma. ATLS®: Advanced Trauma Life Support Student Course Manual. 2018.
- Branney SW, Wolfe RE, Moore EE, et al. Quantitative Sensitivity of Ultrasound in Detecting Free Intraperitoneal Fluid: J Trauma: Injury, Infect Crit Care. 1995;39(2):375-380.
- Stengel D, Bauwens K, Sehouli J, et al. Discriminatory power of 3.5 MHz convex and 7.5 MHz linear ultrasound probes for the imaging of traumatic splenic lesions: A feasibility study: J Trauma: Injury, Infect Crit Care. 2001;51(1):37-43.
- Blackbourne LH, Soffer D, McKenney M, et al. Secondary ultrasound examination increases the sensitivity of the FAST exam in blunt trauma: J Trauma: Injury, Infect Crit Care. 2004;57(5):934-938.
- Muradali D, Wilson S, Burns PN, et al. A specific sign of pneumoperitoneum on sonography: enhancement of the peritoneal stripe. AJR Am J Roentgenol. 1999;173(5):1257-62.
- Chao A, Gharahbaghian L, Perera P. Diagnosis of pneumoperitoneum with bedside ultrasound. West J Emerg Med. 2015;16(2):302.
Zoe Grabinski, MD
Pediatric Emergency Medicine Fellow, Columbia University Medical Center
Joni Rabiner, MD
Pediatric Emergency Ultrasound Fellowship Director, Columbia University Medical Center



