Transcranial Doppler in the Emergency Department: A Clinical Application and Quick Reference
Brian Makowski, DO, Cleveland Clinic Akron General
Robert T. Stenberg, MD, FACEP, Cleveland Clinic Akron General
Case Presentation
A middle-aged female presents to your Freestanding Emergency Department for growing confusion throughout the morning. Patient’s husband reports that she was recently discharged home yesterday following a 12-day hospitalization. He reports the patient was initially admitted to the hospital after a brain aneurysm ruptured. Husband states that the patient had been recovering well with only some mild memory issues and had otherwise appeared to be back to her baseline; until this morning.
On arrival, the patient is noted to be minimally responsive, with a GCS of 7, and is emergently intubated for airway protection. You obtain a CT Head and CTA Head/Neck that appear stable and grossly unchanged from her priors before discharge. Results of initial lab workup return without any clinically significant abnormalities. As you continue to consider common complications in the setting of the patient’s recent spontaneous aneurysmal subarachnoid hemorrhage, vasospasm quickly rises to the top of your differential. Given your Freestanding ED’s limited ancillary services, you decide to test your PoCUS abilities and perform Transcranial Doppler at the bedside.
Background
Transcranial Doppler (TCD) Ultrasonography is a non-invasive, rapid, and repeatable technique that allows for real-time assessment of cerebral blood flow velocities. Although a variety of interesting applications exist (midline shift, elevated intracranial pressure, stroke, prognostics for traumatic brain injury, etc.), the use of TCD for evaluation of middle cerebral artery (MCA) vasospasm has been researched the most extensively. When compared to the gold standard of CT angiography, studies have demonstrated TCD to have a sensitivity and specificity between 89 to 98% for diagnosis of subarachnoid hemorrhage (SAH) associated vasospasm.1,2 TCD provides a unique bedside supplement in the evaluation of patients with neurologic emergencies and may be of even more utility in situations of limited resources or patient instability.
Although able to be performed through four different acoustic windows (transtemporal, transoccipital, transorbital, and submandibular), point-of-care TCD is a limited evaluation and performed through the transtemporal window (Figure 1). It is important to note that in approximately 15% of individuals, ultrasound transmission through the temporal bone is not possible due to inadequate acoustic penetration, and a main limitation of bedside TCD.2,3
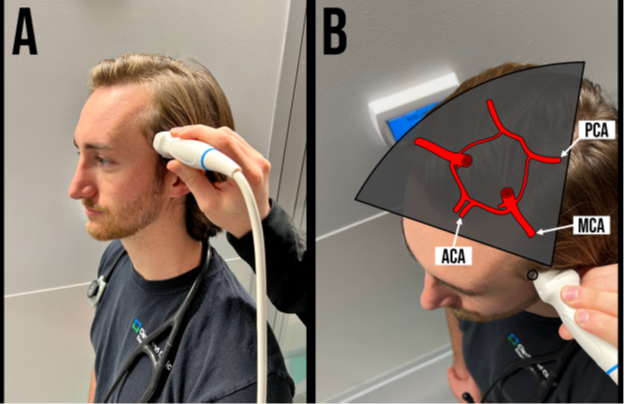 Figure 1. A. Transtemporal transducer positioning B. Transtemporal window and relationship to main cerebral arteries
Figure 1. A. Transtemporal transducer positioning B. Transtemporal window and relationship to main cerebral arteries
TCD ultrasound should be performed with a low-frequency (< 2 MHz) Phased-Array Transducer, and if no TCD pre-set is available, the Cardiac pre-set can be used. To obtain a transtemporal window, the transducer is placed just superior to the zygomatic arch and anterior to the ear.
The transducer indicator should point towards the ipsilateral eye in the TCD pre-set, or towards the occiput if in Cardiac pre-set (Figure 1). The transducer is then oriented slightly upwards and anteriorly. Key landmarks of the transtemporal window include the hypoechoic, butterfly-shaped, cerebral peduncles, and are surrounded by the echogenic, star-shaped, basal cisterns. Color Doppler is then applied over this area and should reveal the circle of Willis. Multiple segments of the intracerebral vessels are able to be visualized in the transtemporal window, including those of the middle cerebral arteries (MCA), anterior cerebral arteries (ACA), and posterior cerebral arteries (PCA) (Figure 1 & 2). Pulsed-Wave Doppler is then applied with the gate placed through the ipsilateral MCA, which appears as a red color doppler signal traveling towards the probe. The normal spectral waveform of the MCA includes the following characteristics: a sharp systolic upstroke and a stepwise diastolic deceleration with positive end-diastolic flow. (Figure 2)
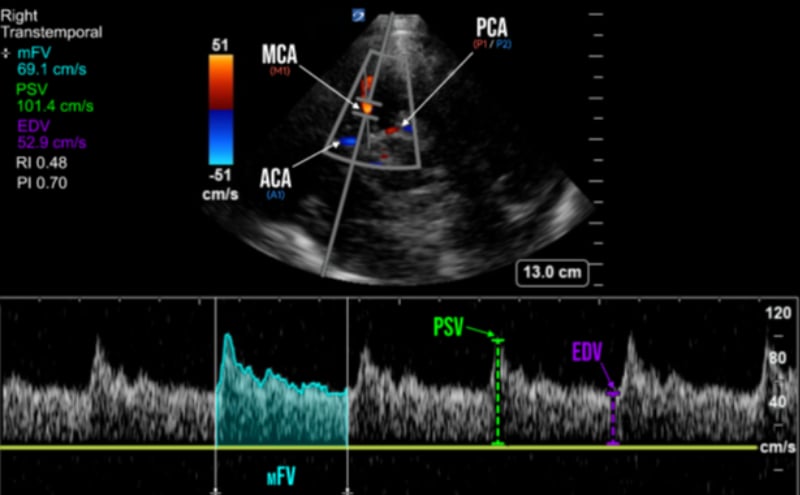
The primary parameter of TCD is known as the Mean Flow Velocity (mFV) (which is also called Time Average Mean, or TAM). MCA Vasospasm is defined by a mFV >120 cm/s, with severity further categorized as mild (>120 cm/s), moderate (>150 cm/s), and severe (>200 cm/s).1,3 mFV is calculated through measurement of the Peak-Systolic Velocity (PSV) and End-Diastolic Velocity (EDV) on spectral doppler, however some ultrasound machines are capable of automatic calculation of the mFV by tracing of the spectral doppler waveform (Figure 2).
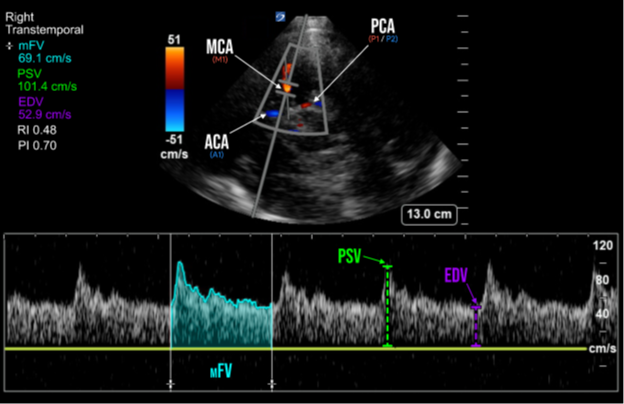
Figure 2. Spectral doppler of the middle cerebral artery (MCA) and its measured parameters In addition to vasospasm, other pathologies causing cerebral hyperemia from global hyperdynamic blood flow (sepsis, fever, anemia, hypercapnia, etc.) can also increase MCA mFV. Further differentiation can be accomplished through calculation of the Lindegaard ratio, which is simply a ratio of the MCA mFV divided by the ipsilateral extracranial internal carotid artery (ICA) mFV. The Lindegaard ratio can thus not only help with differentiation between hyperemia and vasospasm, but is also another method of quantifying vasospasm severity.
Case Resolution
After performing your bedside scan, you note the patient's MCA mFV to be >200 cm/s and subsequently find a Lindegaard ratio of >6, only further raising concerns for post-SAH vasospasm. You quickly begin to arrange transport of the patient to a tertiary care facility with neurosurgical services and additionally contact the on-call neuro-interventionalist for definitive care of your suspected diagnosis.
Discussion
Point-of-Care TCD provides a rapid, non-invasive evaluation for the critical diagnosis of vasospasm and can potentially expedite the patient’s time to definitive care. Delayed cerebral ischemia secondary to vasospasm is a frequent complication after SAH, and has been shown to significantly increase morbidity and mortality.4 The ability to recognize vasospasm on bedside PoCUS can thus facilitate arranging both neurosurgical and neuro-interventional evaluations and help guide a patient’s course to definitive care measures. Recent studies have shown increasingly shorter hospital courses in post-aneurysmal SAH patients with mean length of stays as short as 6.6 to 15 days.5 Incidence of vasospasm has been found to occur typically between 4 and 21 days after initial bleed. When taking both these factors into consideration, it is a practical scenario that patients could vasospasm after discharge and subsequently return to the emergency department. Point-of-Care TCD provides emergency physicians with yet another diagnostic tool in their sonographic toolbox for rapid diagnosis and treatment of patients.
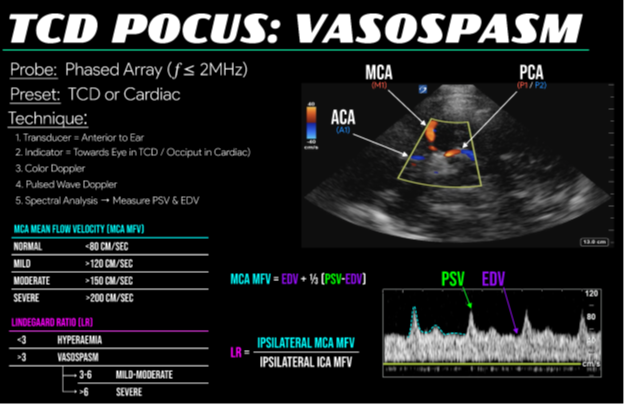
Figure 3. Illustration and quick reference card for point-of-care transcranial doppler
References
- Montrief T, Alerhand S, Jewell C, Scott J. Incorporation of Transcranial Doppler into the ED for the neurocritical care patient. Am J Emerg Med. 2019;37(6):1144-52. doi:10.1016/j.ajem.2019.03.003
- EMCrit A. Neuro-Ultrasound - EMCRIT Project. EMCrit Project. Published February 10, 2023. https://emcrit.org/ibcc/sono/
- Blanco P, Blaivas M. Applications of Transcranial Color-Coded Sonography in the Emergency Department. J Ultrasound Med. 2017;36(6):1251-66. doi:10.7863/ultra.16.04050
- Macdonald RL, Hunsche E, Schüler R, Wlodarczyk J, Mayer SA. Quality of life and healthcare resource use associated with angiographic vasospasm after aneurysmal subarachnoid hemorrhage. Stroke. 2012;43(4):1082-88. doi:10.1161/STROKEAHA.111.634071
- Collins CI, Hasan TF, Mooney LH, et al. Subarachnoid Hemorrhage "Fast Track": A Health Economics and Health Care Redesign Approach for Early Selected Hospital Discharge. Mayo Clin Proc Innov Qual Outcomes. 2020;4(3):238-48. Published 2020 Jun 5. doi:10.1016/j.mayocpiqo.2020.04.001
Additional Resources
CoreUltrasound: 5 Minute Sono – Neuro
EMRA: Can Transcranial Doppler Be Useful in the ED? A Review of the Literature
Western Sono: Transcranial Doppler (TCD)
EMCrit IBCC: Neuro-ultrasound
Ultrasound G.E.L. Podcast: Transcranial Doppler in Traumatic Brain Injury



