ACEP's First Take from the Combined 2024 Medicare Physician Fee Schedule (PFS) and MACRA Quality Payment Program (QPP) Final Rule
On November 2, 2023, the Centers for Medicare & Medicaid Services (CMS) released a Medicare annual final payment rule for calendar year (CY) 2024 that impacts payments for physicians and other healthcare practitioners. The rule combines policies for the Medicare physician fee schedule (PFS) with those for the Merit-based Incentive Payment System (MIPS)—the quality performance program established by the Medicare Access and CHIP Reauthorization Act (MACRA). The final rule finalizes most of the proposals included in the CY 2024 PFS proposed rule released on July 13, 2023. ACEP submitted a comprehensive response to that proposed rule on September 11, 2023.
Below is a high-level summary of key policies separated by proposed PFS and MIPS policies.
Physician Fee Schedule
CMS has finalized a CY 2024 Resource-Based Relative Value Scale (RBRVS) Conversion Factor (CF) of $32.7375, which represents an approximately 3.39% reduction from the final CY 2023 RBRVS CF of $33.8872. The final CF for Anesthesia is $20.4349, representing an approximately 3.27% reduction from the final CY 2023 Anesthesia Conversion Factor of $21.1249. The finalized CF update is primarily based on three factors: a statutory 0% update scheduled for the Physician Fee Schedule (PFS) in CY 2024, a negative 2.20% budget neutrality adjustment, and a funding patch passed by Congress at the end of CY 2022 through the Consolidated Appropriations Act, 2023, which partially mitigated a cut to the CY 2023 CF and offset part of the reduction to the CY 2024 CF.
Concerning other proposed spending increases, CMS is not only phasing in the third year of a clinical labor pricing update, but in addition, CMS has decided to maintain its previous policy to add G2211, an add-on code for complexity. As background, CMS had finalized this new add-on code in the CY 2021 PFS Final Rule, but it carried large budget neutrality implications because CMS estimated G2211 would be billed with 90% of all office visit claims. This was expected to redistribute around $3.3 billion and cause a 3% cut to the CF for 2021. In December 2020, Congress passed the Consolidated Appropriations Act 2021, which delayed G2211 until 2024. Now, CMS has finalized their decision to reinstate it. CMS revised their utilization assumption from 90% in the 2021 PFS to 38% in the 2024 PFS proposed rule. CMS finalized this 38% utilization assumption in the final rule.
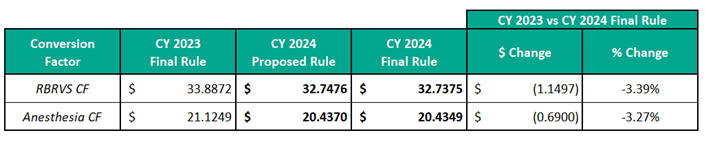
Initially, CMS had proposed a 3.36% reduction from the final CY 2023 RBRVS Factor and a 3.26% reduction from the final CY 2023 Anesthesia Conversion Factor. While this final rule represents a slightly increased reduction over the proposed, Congress is still considering potential relief in an end-of-year legislative package. However, it is still unclear if lawmakers can fully offset these final payment reductions.
- Split or Shared Services: In the CY 2022 PFS final rule, CMS finalized a policy for determining whether a physician or non-physician practitioner should bill for an E/M service they both were delivering (called split/shared services). Under Medicare, a service can only be billed by one clinician, and if non-physician practitioners wind up billing for a service, they only receive 85 percent of the total Medicare rate.
The finalized policy from the CY 2022 final rule applies only to E/M services delivered in facilities (including the ED)—and excludes critical care. The key here is deciding who provides the "substantive" portion of the service. CMS decided to phase in the policy — in 2022, the history, physical exam, medical decision making (MDM), or more than half of the total time spent with a patient, can be used to determine the substantive portion of the split/shared visit. However, going forward, only time would be used to determine the substantive portion of a split/shared visit.
ACEP, the American Medical Association (AMA), and many other specialty societies strongly oppose using only time to determine the substantive portion of a split/shared E/M service and formally requested that CMS reverse its 2023 policy in the upcoming reg and instead modify it to allow the determination to be made based on time OR MDM.
In last year's proposed rule, CMS proposed to delay the implementation of the full transition to time only until 2024. However, in light of comments CMS received, CMS is finalizing a policy that reflects a revised definition of the "substantive portion" of a split (or shared) visit to reflect the revisions to the CPT E/M guidelines, such that for Medicare billing purposes, the "substantive portion" means more than half of the total time spent by the physician and NPP performing the split (or shared) visit, or a substantive part of the medical decision making except concerning critical care visits which do not use MDM and only use time, "substantive portion" continues to mean more than half of the total time spent by the physician and NPP performing the split (or shared) visit. CMS notes that it is finalizing this policy for CY 2024, in part, to avoid the administrative burden described by commenters that would otherwise be present for facilities and practices that spend time and resources preparing for potential policy changes that are delayed year after year.
- Telehealth: CMS is finalizing its proposal to reform the current process for adding new services to the Medicare Telehealth List. Currently, CMS adds services to the list based on two permanent categories (Categories 1 and 2) and one temporary category (Category 3). The temporary category was established during the COVID-19 public health emergency, and the plan was to eventually eliminate Category 3 and assess whether the services temporarily added to the list during the PHE should be permanently added based on a Category 1 or Category 2 review. Services added to the Medicare Telehealth List on a Category 1 basis are similar to those already permanently on the list, such as office-based services. Category 2, which applies to non-office-based services, involves a review of peer-reviewed literature that proves whether the service, when provided via telehealth, improves quality and reduces costs. CMS is finalizing its proposal to eliminate the three categories and replace them with a unified process for adding new codes to the Medicare Telehealth List, either temporarily or permanently
In this rule, CMS decides to maintain ED E/M levels 1-3 and some observation codes on the list of approved telehealth services at least through the end of CY 2024:
- ED E/M Codes Levels 1-3: 99281-99283
- Initial Hospital Inpatient or Observation Care - 99221-99223
- Hospital Inpatient or Observation Care Services, Same Day Admission and Discharge - 99234-99236
- Discharge from Hospital Inpatient or Observation Care - 99238-99239 Other telehealth policies include:
- Allowing the higher non-facility payment rate for telehealth services performed for patients at their homes. These services would be billed under the place of service (POS) code 10. However, CMS will return to its pre-pandemic policy of paying the lower facility-based rate for all telehealth services where patients are not at home.
- Temporary expansion of the telehealth originating sites for any service on the Medicare Telehealth Services List to include any site in the United States where the beneficiary is located at the time of the telehealth service, including an individual's home, beginning on the first day after the end of the PHE for COVID-19 through December 31, 2024;
- Continuation of the definition of "direct supervision" to permit the presence and "immediate availability" of the supervising practitioner through real-time audio and visual interactive telecommunications through December 31, 2024;
- Allowing teaching physicians to use audio/video real-time communications technology when the resident furnishes Medicare telehealth services in all residency training locations through the end of CY 2024.
- Appropriate Use Criteria Program: In a victory for emergency physicians and their patients, CMS has officially canceled the Appropriate Use Criteria (AUC) Program. CMS has continuously delayed the program, and ACEP had previously requested that CMS work with Congress to repeal the program. We have argued that the program is unnecessary and could harm patient care by postponing vital treatment.
As background, the AUC program would have required clinicians to consult appropriate use criteria using clinical decision support tools before ordering advanced imaging services for Medicare beneficiaries. While an exception for emergency medical conditions exists, ACEP had heard that some hospitals have not appropriately updated their systems to allow emergency physicians to claim the exception. This had caused confusion and fear that emergency physicians, despite the noted exception, would still have to consult appropriate use criteria even during suspected or confirmed medical emergencies, wasting valuable time.
CMS is pausing implementation of the AUC program for reevaluation and rescinding the current AUC program regulations. CMS expects this to be a hard pause to facilitate thorough program reevaluation and is not establishing a time frame within which implementation efforts may recommence.
- The Medicare Shared Savings Program: The Medicare Shared Savings Program is the national Accountable Care Organization (ACO) program, which serves over 11 million people with Medicare. In the rule, CMS is finalizing numerous changes to the program, including:
- Making changes to the quality reporting requirements;
- Modifying how beneficiaries are assigned to ACOs;
- Seeking comment on MIPS Value Pathways (MVPs) for specialists in ACOs;
- Modifying the benchmark
- Opioid Treatment Programs (OTPs): CMS is extending current flexibilities for certain assessments furnished via audio-only telecommunications through CY 2024.
- Requirement for Electronic Prescribing for Controlled Substances for a Covered Part D Drug under a Prescription Drug Plan or an MA-PD plan: CMS is continuing to implement a provision of the Substance Use Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities (SUPPORT) Act, which requires electronic prescribing of controlled substances (EPCS) under Medicare Part D. In the rule, CMS states that the agency will continue its current policy of not instituting any financial penalties for non-compliance. CMS will issue a notice of non-compliance as a non-compliance action for the foreseeable future.
- Dental and Oral Health Services: In last year's rule, CMS finalized expanded payment for dental services. In this year's rule, CMS is codifying the previously finalized payment policy for dental services.
Quality Payment Program
CMS finalizes policies that impact the seventh performance year (2023) of the Quality Payment Program (QPP). The QPP includes two tracks: the Merit-based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (APMs). MIPS includes four performance categories: Quality, Cost, Improvement Activities, and Promoting Interoperability (formally Meaningful Use). Performance on these four categories (weighted) rolls up into an overall score that translates to an upward, downward, or neutral payment adjustment that providers receive two years after the performance period (for example, performance in 2024 will impact Medicare payments in 2026).
- 2023 Reporting Exemptions Due to COVID-19: As described here, CMS is granting hardship exemptions on a case-by-case basis due to COVID-19. Therefore, a clinician or group can request to be exempted from all four performance categories in If clinicians submit a hardship exception application for all four MIPS performance categories, and their application is approved, they will be held harmless from a payment adjustment in 2025—meaning that they will not be eligible for a bonus or potentially face a penalty based on their MIPS performance in 2023.
- MVPs: The 2024 performance year is the second year in which a new reporting option in MIPS called MIPS Value Pathways (MVPs) is available. MVPs represent an approach allowing clinicians to report on a uniform set of measures on a particular episode or condition to get MIPS ACEP developed an emergency medicine-focused
MVP that CMS included in the first batch of MVPs that began this year.
In this year's rule, CMS is finalizing its proposal to add three new MIPS quality measures and one QCDR measure to the emergency medicine-focused MVP. CMS is also adding one improvement activity and removing another. Concerning the cost category, CMS is removing the Medicare Spending Per Beneficiary (MSPB) Clinician measure and adding the emergency medicine cost measure, as described below.
Please click here for more information about the MVP option, including registering for the MVP in 2023.
- Performance Category Weighting in Final Score: CMS will maintain the same performance category weights as in 2023. The weights are required by law.
General Performance Category Weights Proposed for 2024:
- Quality: 30%
- Cost: 30%
- Promoting Interoperability (EHR): 25%
- Improvement Activities: 15%
- Performance Threshold: CMS is NOT finalizing its proposal to increase the threshold clinicians need to achieve to avoid a penalty to 82 points in 2024 and is maintaining its 75-point performance threshold. By law, CMS has to set the performance threshold at the mean or median of a prior performance year, and the agency decided to pick the 2019 performance period when setting the 2024 performance threshold. ACEP had opposed the proposal to raise the threshold and had encouraged CMS to keep the threshold at 75 points.
As a reminder, there is no exceptional bonus threshold starting in the 2023 performance period. The 2022 performance period (which impacts payments in 2024) was the last year the additional funding for exceptional performance was available.
- Qualified Clinical Data Registries (QCDRs): ACEP owns and operates its own QCDR, the Clinical Emergency Data Registry (CEDR). In the rule, CMS is finalizing several new requirements for QCDRs.
- Emergency Medicine Cost Measure: CMS' contractor, Acumen, convened a workgroup to develop an emergency medicine episode-based cost measure. ACEP nominated a few individuals to serve on that workgroup, and we are pleased that three ACEP members participated in it—including the workgroup chair. The emergency medicine cost measure will be incorporated into the MIPS program 2024.
- Other MIPS Proposals:
- Maintain its previous proposal to increase the data completeness criteria threshold from 70 percent to 75 percent for the CY 2024 and 2025 performance periods and set the data completeness threshold at 75 points for the CY 2026 performance period (CMS did not finalize its proposal to raise the data completeness threshold to 80 points in CY 2027)
- Maintain the inventory of quality measures at 198 through the addition of 11 and the removal of 11 MIPS quality measures (a net of zero);
- Add five new episode-based cost measures (including the emergency medicine cost measure);
- Add 5 new improvement activities, modify 1 existing improvement activities, and remove 3 existing improvement activities for a total of 106 in the MIPS inventory;
- Increase the performance period to a minimum of 180 continuous days within the calendar year;
- Clarify that if a facility-based clinician reports through an MVP, CMS will take the higher of the MVP score and the score the clinician receives through facility-based measurement.
- Advanced APMs: CMS is NOT finalizing its proposal to make the Qualifying APM Participant (QP) determinations at the individual eligible clinician level only instead of the APM Entity level. ACEP had opposed this proposal.
Clinicians with a certain proportion of their revenue or patient population tied to an Advanced APM (known as the revenue or patient threshold) are classified as a QP, eligible for a bonus, and exempt from MIPS. As required by statute, CMS is increasing those thresholds in 2024.
Author(s)

Erin Grossman
Regulatory and External Affairs Manager
Author(s)

Aarti Gupta MBBS
CEDR Account Manager
 American College of Emergency Physicians
American College of Emergency Physicians